New research from The University of Toledo’s College of Medicine and Life Sciences may give patients suffering from inflammatory bowel disease a better roadmap for managing their symptoms by changing the type of fiber they eat during flare-ups.
Because there’s no cure for the chronic condition, patients living with Crohn’s disease and ulcerative colitis — the two most common types of inflammatory bowel disease (IBD) — often rely on anti-inflammatory or immunosuppressive drugs and careful diet planning to manage their symptoms, said Dr. Matam Vijay-Kumar, the senior author on the study and director of the UT Microbiome Consortium and associate professor in the UT Department of Physiology and Pharmacology.
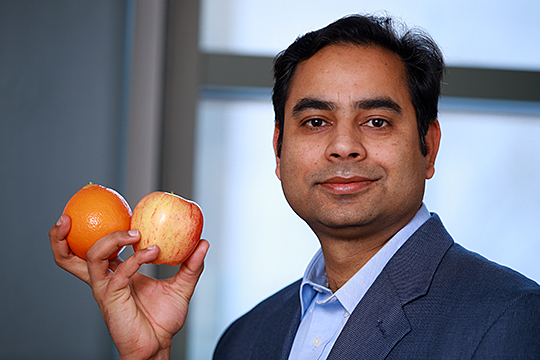
Research conducted by Dr. Vishal Singh suggests foods high in the dietary fiber pectin, found in apples and extractable from orange peels, may help individuals with inflammatory bowel disease.
“IBD can be a debilitating condition and its prevalence is on the rise. For IBD patients, there has been a puzzling question of why they report poor tolerance to certain types of dietary fibers,” said Dr. Vishal Singh, a Crohn’s and Colitis Foundation Fellow mentored by Vijay-Kumar at UT.
“For healthy people, dietary fibers are good,” he said. “But when it comes to the IBD patients, not all-natural fibers are created equal; thus, their metabolism is distinct. We wanted to understand why.”
In a study published last month in the gastroenterology journal Gut, a team of UT researchers demonstrated a diet rich in pectin or pectin-derived fibers may be a better alternative to the prevailing dietary fiber guidelines aimed at helping patients improve their IBD symptoms.
The study also confirmed that inulin and inulin-like fiber exacerbated colitis in lab mice.
Inulin and pectin are two of the most common refined fibers added to processed foods as a way to add texture and boost their health appeal. Both are indigestible soluble fibers, Vijay-Kumar said, but they require different bacterial enzymes to be broken down in the gut into short-chain fatty acids.
“Many patients try to avoid fiber,” said Singh, the study’s first author. “However, the research shows it’s not about reducing fiber in general, but getting the right kind into your system.”
Singh and his fellow researchers said the finding could assist patients in developing a better diet for managing or preventing flare-ups.
“Following strict dietary guidelines is not new for IBD patients. Physicians often recommend patients limit or avoid a group of foods that contain fermentable carbohydrates, commonly known as the low-FODMAP diet,” Vijay-Kumar said. “Pectin is not included in that diet, but our research shows it brings a clear benefit.”
The study was supported by the Crohn’s and Colitis Foundation, and the National Cancer Institute of the National Institutes of Health.
In the study, researchers examined the role played by bacteria that naturally reside in the gut. They demonstrated that inulin promoted accelerated growth of one particular harmful bacterial strain, while pectin did not.
They also found that a brief period of fasting may boost the body’s production of a physiological inflammation inhibitor that can protect against the inflammatory reaction caused by the gut bacteria processing inulin.
“For me, this study connects very well from bench to bedside,” Singh said. “If an IBD patient is noticing complications after eating some type of food, they can look to see if it is rich in inulin or inulin-type fibers. If it is, they can switch to foods enriched with pectin.”
Pectin is found naturally in a variety of foods, including apples. It also can be derived from other natural sources, such as orange peels, and used as a food additive.
Though the study looked only at pectin and inulin, the team hopes to conduct similar studies on a wide variety of dietary fibers present in processed foods with the goal of learning more about how different types of fiber cause or reduce colonic inflammation.