The deck is stacked against those facing a pancreatic cancer diagnosis, with the latest data showing a five-year survival rate under 13%.
The reasons for that grim fact are many, but among them is the challenge clinicians face in treating the cancer. Surgery is not always an option, and pancreatic cancer cells are notoriously difficult to reach with drugs.
Dr. Shi-He Liu, an assistant professor of cell and cancer biology, received a $2.5 million grant to develop a new drug delivery method for pancreatic cancer.
“The problem is not so much about finding a way to kill the cancer cells,” said Dr. Shi-He Liu, a cancer researcher at The University of Toledo. “It’s about finding a way to effectively deliver therapeutic agents to those pancreatic cancer cells.”
Liu has a theory on how to do that better.
The assistant professor of cell and cancer biology recently received a $2.5 million, five-year grant from the National Cancer Institute to continue his exploration of using genetically engineered exosomes as nanocarriers to deliver drugs directly to cancer cells that carry specific surface biomarkers.
You can think of exosomes kind of like a microscopic fleet of Amazon vans working the space between cells in our body.
The exosomes, which are secreted by almost all human cells, carry proteins and genetic information from one cell to another, providing essential intercellular communication and cellular signaling. Because of that function, they’re an appealing area of research for drug delivery.
“Naturally they have a function of transportation. We’re trying to take advantage of that,” Liu said.
However, the challenge with natural exosomes is directing them to deliver their payload to exactly the right spot and enabling them to circulate long enough to reach their destination. Natural exosomes lack the ability to actively target tumor cells and are rapidly attacked and cleared by the immune system.
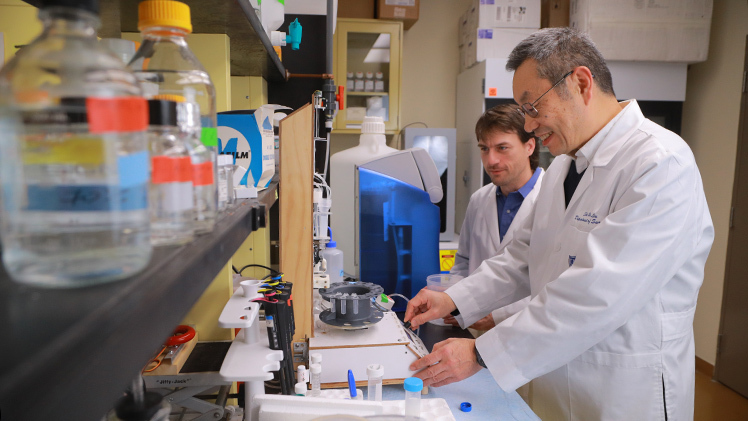
To overcome those hurdles, Liu’s team has genetically engineered exosomes, called “smart exosomes,” to home in on pancreatic tumor cells and be recognized by the immune system as a friendly passerby — not a potential threat.
With the five-year grant from the National Cancer Institute, Liu will continue researching novel approaches to targeting pancreatic cancer therapies.
“If not for the engineering, they’d go everywhere and quickly be cleared by the body’s macrophage system,” he said. “What we’re doing is almost like putting a magnet on those structures that attract them to the cancer cells while pushing them away from the immune cells.”
The group’s preliminary data has been strong, with the engineered exosomes showing they can successfully target cancer cells while sending a “don’t eat me” signal to the macrophages.
With the latest federal funding, UToledo researchers will continue laboratory studies and expand the scope of their investigation to testing the drug delivery system in animal models. In addition to validating the concept, they’re also aiming to develop a library of smart exosomes that could match a wide variety of pancreatic tumor biomarkers.
Initially Liu is loading the engineered exosomes with standard, first-line treatments, though he and his collaborators also are working to develop new small molecule therapies.
“The big thing in cancer care right now is precision medicine. For pancreatic cancer, there has been little benefit from the current precision medicine and immune-based therapies,” he said. “It’s an area that’s not easily reached, but we hope we can overcome that and one day provide better outcomes for patients with pancreatic cancer.”
Co-investigators on the project include Dr. Jian-Ting Zhang, professor and chair of the Department of Cell and Cancer Biology, and Dr. Yakov Lapitsky, a professor of chemical engineering.