Scientists in The University of Toledo College of Medicine and Life Sciences are launching a new study of acute lung injury that will, in part, investigate repurposing a common asthma medication as a new way to treat the serious and often deadly condition brought on by excessive inflammation.
The project, led by Dr. Sailaja Paruchuri, is being funded by a four-year, $2.32 million grant from the National Institutes of Health.
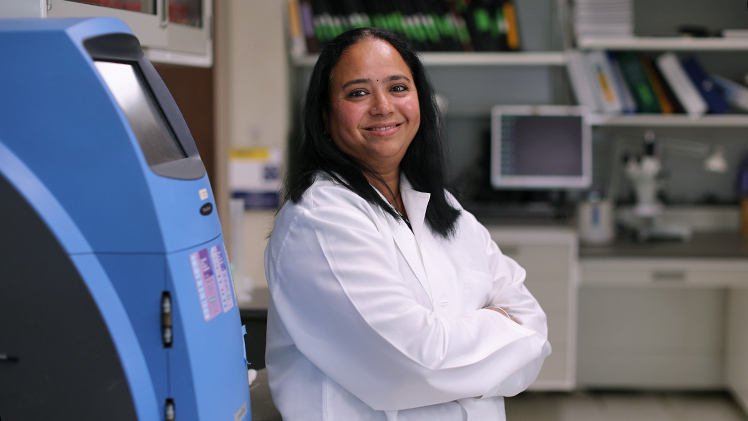
Dr. Sailaja Paruchuri, a professor in the Department of Physiology and Pharmacology, is leading the NIH-funded project that will look at repurposing an existing asthma medication to treat acute lung injury.
Our lungs are exposed to all sorts of airborne pathogens. Some are more dangerous than others, but they all evoke an immune response. Ideally, that immune response clears out the contaminants and allows the lungs to heal.
Sometimes, however, our immune cells don’t get the message that the battle is over.
“If you have a bacterial infection in your lungs, your doctor might prescribe you antibiotics to clear away the bacteria. Often, that’s the end of it,” said Paruchuri, a professor in the Department of Physiology and Pharmacology. “In acute lung injury, however, the real damage is being done by an overactive immune system. The bacteria may be gone, but that runaway immune response can quickly cause organ damage and ultimately a failure to breathe.”
Not everyone who has a lung infection ends up with acute lung injury, but among the 200,000 annual cases in the United States, up to 40% are fatal.
Paruchuri’s research is focused on cysteinyl leukotrienes — a specific kind of lipid that mediates inflammation. You can think of it something like a toggle switch that activates and deactivates the body’s immune response.
Those molecules are particularly well known for causing allergic inflammation and their role in asthma. The FDA-approved medication Singulair, for example, manages asthma symptoms by blocking receptors that recognize cysteinyl leukotrienes.
Paruchuri’s lab, however, discovered that those inflammatory lipid mediators also act on macrophages, a specialized type of white blood cell.
From left, Dr. Sailaja Paruchuri, a professor in the Department of Physiology and Pharmacology and lab members: Dr. Lakshminarayan Reddy Teegala, an assistant professor in the Department of Physiology and Pharmacology; and doctoral students Emma Elizabeth Sabu-Kattuman and Somayeh Darzi.
“Macrophages are very interesting defense cells because they have this ability to become both pro-inflammatory and anti-inflammatory. Everything depends on the signal they get,” Paruchuri said. “If there is a bacterial infection, those cells get a signal to become warriors. When the infection is done, they get signals to go from warriors to scavengers and clean up the battlefield.”
The trouble comes when that stand-down message doesn’t go through — leading them to continue their attack.
“You need that immune response to clear out the infection, but too much of a response can be harmful,” she said. “In some patients, there’s a dysregulation in macrophages that’s making them too stimulated.”
Based on her preliminary work, Paruchuri believes cysteinyl leukotrienes receptors may be the key to the imbalance seen in acute lung injury.
In the new study, which is funded through the National Heart, Lung and Blood Institute, Paruchuri and her colleagues will aim to broadly understand the role cysteinyl leukotrienes receptors play in acute lung injury, as well as determining exactly how those receptors are activated on macrophages and what signals are being sent into the cells to direct them toward pro- or anti-inflammatory action.
Crucially, they also will investigate whether Singulair could be repurposed as a novel treatment for patients with acute lung injury.
Because that medication acts to block the same kind of receptors Paruchuri and her team have identified as playing a role in acute lung injury, there is hope it might prove to be an effective treatment
“If we can identify the signals which make the macrophages super active and make the situation worse, then we can think of getting better therapeutic options,” Paruchuri said. “When a patient comes with acute lung injury, we don’t use Singulair for that. But in the future, if our project works as we anticipate, maybe we can extend that drug to treat acute lung injury.”