How dangerous illicit drugs like heroin affect our bodies and minds is well understood.
The same cannot be said for the increasingly popular lab-created psychoactive agents that have flooded the market over the last decade.
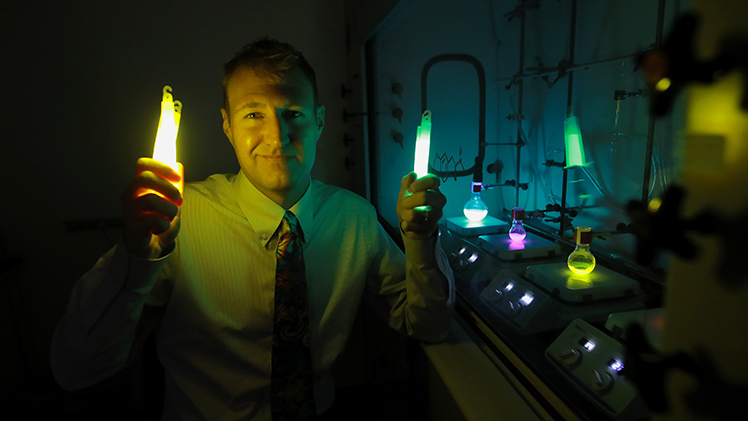
Dr. Isaac Schiefer, a professor of medicinal and biological chemistry and Director of the Center for Drug Design and Development in the College of Pharmacy and Pharmaceutical Sciences, is leading research to better characterize the mechanisms behind street drugs with a long-term goal of combating their toxicity and potentially identifying future therapeutic uses.
“Not only do these designer drugs often fly under the radar of regulators, but scientists don’t entirely understand how they work or what contributes to the toxicity that we see in many of them,” said Dr. Isaac Schiefer, a professor of medicinal and biological chemistry and Director of the Center for Drug Design and Development in The University of Toledo College of Pharmacy and Pharmaceutical Sciences.
An expert in central nervous system drug discovery, Schiefer is leading new federally funded research to better characterize the mechanisms behind those street drugs with a long-term goal of combatting their toxicity and potentially identifying future therapeutic uses.
Often created at an industrial level in overseas laboratories, the drugs UToledo researchers are studying — known as bath salts — can be strong stimulants or mind-altering hallucinogens. In some cases, the same drug can be either one, or both, depending on the dose someone takes.
Not only are the drugs ubiquitous, but they also are constantly changing as drug manufacturers tweak their chemical formulas to circumvent new laws and regulations.
The result is an ever-evolving library that includes hundreds if not thousands of illicit substances, each with their own unique properties.
“Very small structural changes lead to huge differences in toxicity and how the drugs affect our perception of reality,” Schiefer said. “We are going to look at the molecular level to figure out what the targets are that are responsible for these actions, why are some hallucinogenic, why are some stimulants, why are some empathogens and why certain ones are toxic to see if we can connect the dots as to what’s happening within the class.”
The $2.65 million grant from the National Institute on Drug Abuse builds on Schiefer’s earlier work to develop a new way of determining the specific protein targets of drugs using a tried-and-true method called photoaffinity labeling.
Photoaffinity labeling, which uses ultraviolet light to freeze and characterize the binding targets of molecules, is widely employed in drug discovery but its use has been limited to looking at cells outside the body.
Schiefer wanted to take that process a step further and be able to see those interactions in live organisms themselves.
Using a specially bred translucent zebrafish, Schiefer and colleagues demonstrated the ability of UV light to penetrate tissues, allowing for the real-time identification of drug targets in the living animals.

Using a specially bred translucent zebrafish, Schiefer can study real-time identification of drug targets in the living animals.
“Because these fish lack pigmentation, it allows us to use UV light to manipulate the chemistry in the brain,” he said. “This is the first example of a target identification platform where you can actually look at what a drug was bound to when a behavioral change was observed.”
That proof-of-concept research, which was published two years ago in the journal ACS Chemical Neuroscience, served as the basis for his new grant.
With the new platform, Schiefer and his collaborators will use a combination of chemical probes — small molecules designed to look like a specific psychoactive agent — alongside tiny amounts of the drugs themselves to zero in on the specific protein targets responsible for the altered mental state the drugs produce.
The new knowledge Schiefer’s work produces could potentially lead to the development of new molecules to treat individuals suffering from severe reactions after taking club drugs.
“These drugs don’t get regulated or tested. Until we understand how they function in our brains and the toxicity around them, when someone shows up at the ER after taking one of these substances, you don’t know what to do,” he said. “Once we understand how they work, we might be able to develop a molecule to reverse those negative effects.”
The findings also could be applied to treating post-traumatic stress disorder.
There has been a burgeoning interest in psychedelics as a potential PTSD therapy, with trials of both MDMA and psilocybin, the hallucinogenic compound found in certain mushrooms. While the research into those compounds and other psychoactive agents for PTSD is ongoing, Schiefer said concerns remain about associated toxicity.
By understanding the targets of similar, synthetic party drugs, it might be possible to build new molecules that can target and treat the PTSD without any unwanted effects.